Hot flash triggers are common experiences during menopause, characterized by sudden sensations of intense heat and sweating. Understanding the physiological and hormonal changes that occur during hot flashes is crucial for managing their frequency and severity.
This comprehensive guide explores the common triggers that can induce hot flashes, including temperature changes, stress, certain foods and beverages, and medications. It also discusses lifestyle modifications, medical interventions, and coping mechanisms to help individuals navigate this challenging phase.
Common Triggers of Hot Flashes
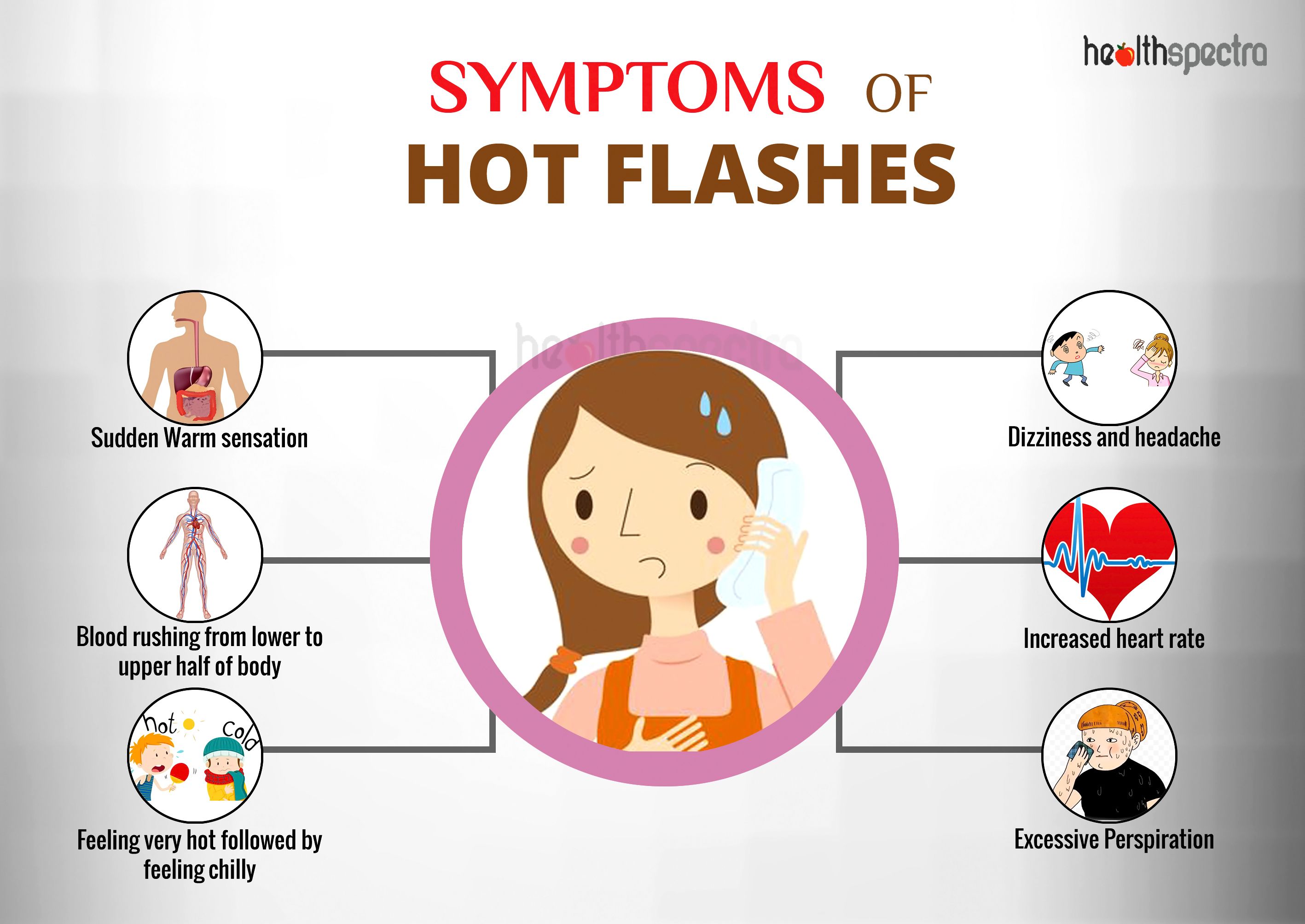
Hot flashes are a common symptom of menopause, characterized by a sudden feeling of intense heat and sweating. While the exact cause of hot flashes is unknown, certain triggers can increase their frequency and severity.
Temperature Changes
Sudden changes in temperature, both hot and cold, can trigger hot flashes. For example, entering a warm room from a cold environment or vice versa can cause the body to react by releasing heat through sweating.
Stress
Stress can be a major trigger for hot flashes. When the body is under stress, it releases hormones such as adrenaline and cortisol, which can increase heart rate and body temperature.
Certain Foods and Beverages
Certain foods and beverages can trigger hot flashes in some individuals. These include:
- Spicy foods
- Alcohol
- Caffeine
- Hot drinks
Medications
Some medications can also trigger hot flashes as a side effect. These include:
- Hormone replacement therapy (HRT)
- Antidepressants
- Steroids
Lifestyle Modifications for Managing Triggers

To effectively manage hot flashes, it is crucial to adopt certain lifestyle modifications that can reduce their frequency and severity.
These lifestyle changes include maintaining a cool environment, managing stress levels, avoiding trigger foods and beverages, and considering alternative therapies such as acupuncture and yoga.
Maintaining a Cool Environment
Maintaining a cool environment can help reduce the frequency and severity of hot flashes. This can be achieved by:
- Keeping the temperature of your home or office cool.
- Wearing loose, breathable clothing made from natural fibers like cotton.
- Taking cool showers or baths.
- Using fans or air conditioning to circulate air.
- Spending time in cool places, such as near a fan or in an air-conditioned room.
Benefits:
- Reduces the risk of triggering hot flashes.
- Provides a sense of comfort and relief.
- Improves sleep quality.
Limitations:
- May not be feasible in all environments.
- Can be expensive to maintain a cool temperature.
Managing Stress Levels
Stress can trigger hot flashes. Managing stress levels can help reduce their frequency and severity.
Some effective stress management techniques include:
- Exercise
- Yoga
- Meditation
- Deep breathing exercises
- Spending time in nature
- Talking to a therapist
Benefits:
- Reduces the frequency and severity of hot flashes.
- Improves overall well-being.
- Helps manage other symptoms of menopause, such as mood swings and anxiety.
Limitations:
- May require time and effort to implement.
- May not be effective for everyone.
Avoiding Trigger Foods and Beverages
Certain foods and beverages can trigger hot flashes. Identifying and avoiding these triggers can help reduce their frequency and severity.
Common trigger foods and beverages include:
- Spicy foods
- Caffeine
- Alcohol
- Sugary drinks
Benefits:
- Reduces the frequency and severity of hot flashes.
- Improves overall health.
- Can help manage other symptoms of menopause, such as weight gain and fatigue.
Limitations:
- May require dietary changes.
- May not be effective for everyone.
Considering Alternative Therapies
Alternative therapies, such as acupuncture and yoga, may help reduce the frequency and severity of hot flashes.
Acupuncture involves the insertion of thin needles into specific points on the body. It is believed to stimulate the release of endorphins, which have pain-relieving and mood-boosting effects.
Yoga is a mind-body practice that combines physical postures, breathing exercises, and meditation. It is believed to reduce stress, improve circulation, and promote relaxation.
Benefits:
- May reduce the frequency and severity of hot flashes.
- Can improve overall well-being.
- May help manage other symptoms of menopause, such as mood swings and anxiety.
Limitations:
- May not be effective for everyone.
- May require time and effort to implement.
Medical Interventions for Trigger Management: Hot Flash Triggers
Medical interventions can provide effective relief from hot flashes for many women. These interventions include hormone replacement therapy (HRT), selective serotonin reuptake inhibitors (SSRIs), and gabapentin.
Hormone Replacement Therapy (HRT)
HRT is the most effective treatment for hot flashes. It involves taking estrogen or a combination of estrogen and progestin to replace the hormones that decline during menopause.
HRT can effectively reduce the frequency and severity of hot flashes by up to 80%. It can also improve sleep quality, mood, and bone density.
However, HRT is not suitable for all women. It is contraindicated for women with a history of breast cancer, blood clots, or liver disease.
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs are antidepressants that can also be used to treat hot flashes. They work by increasing the levels of serotonin in the brain, which can help to regulate body temperature.
SSRIs are generally well-tolerated, but they can cause side effects such as nausea, diarrhea, and insomnia.
Gabapentin
Gabapentin is an anticonvulsant medication that can also be used to treat hot flashes. It is thought to work by reducing the activity of certain nerve cells in the brain that are involved in triggering hot flashes.
Gabapentin is generally well-tolerated, but it can cause side effects such as dizziness, drowsiness, and weight gain.
Impact of Hot Flash Triggers on Quality of Life

Hot flash triggers can significantly impact an individual’s quality of life, affecting various aspects of their well-being. These triggers can disrupt sleep, alter mood, and interfere with social interactions, ultimately affecting their overall sense of well-being.
Sleep Disturbances
Hot flashes can lead to sleep disturbances, causing difficulty falling or staying asleep. The sudden onset of heat and sweating can disrupt sleep patterns, resulting in fragmented sleep and reduced sleep quality. Over time, this can lead to daytime fatigue, irritability, and decreased cognitive function.
Mood Changes, Hot flash triggers
Hot flash triggers can also affect mood, leading to increased irritability, anxiety, and depression. The hormonal fluctuations associated with hot flashes can disrupt emotional regulation, making individuals more susceptible to mood swings and emotional instability.
Social Interactions
Hot flashes can interfere with social interactions, causing embarrassment and discomfort. The unpredictable nature of hot flashes can make it difficult to engage in social situations without the fear of experiencing a hot flash. This can lead to social withdrawal and isolation.
Overall Well-being
The cumulative impact of hot flash triggers on sleep, mood, and social interactions can significantly affect an individual’s overall well-being. It can lead to decreased self-esteem, impaired concentration, and a diminished sense of quality of life.
Coping mechanisms and support strategies are essential for individuals experiencing these challenges. These may include lifestyle modifications, such as avoiding triggers, practicing relaxation techniques, and seeking emotional support from family, friends, or support groups.
Answers to Common Questions
What are the most common triggers of hot flashes?
Common triggers include temperature changes, stress, spicy foods, caffeine, and alcohol.
How can I manage hot flashes through lifestyle modifications?
Maintaining a cool environment, managing stress levels, and avoiding trigger foods and beverages can help reduce the frequency and severity of hot flashes.
What medical interventions are available for managing hot flashes?
Hormone replacement therapy (HRT), selective serotonin reuptake inhibitors (SSRIs), and gabapentin are some medical interventions that may be considered.